As the only National Cancer Institute-Designated Comprehensive Cancer Center in Georgia, Winship is a leader in the treatment of lung and other thoracic cancers, conducting innovative research and clinical trials that are transforming how these cancers are identified, treated, and survived.
The radiation oncologists at Emory Proton Therapy Center work with the multidisciplinary Lung cancer team at Winship, which includes experts in thoracic surgery, medical oncology, pulmonology, radiology, pathology, supportive oncology, dieticians, social workers, physical therapy, and cancer rehabilitation. Your radiation oncologist will work closely with these other specialists to customize your thoracic cancer treatment plan and coordinate your care. We can also partner and coordinate with a patient’s existing care team, whether they are across town or around the world.
Proton Therapy for Thoracic Tumors and Cancers
A lung cancer diagnosis can be one of the biggest challenges you and your family will ever face. Our team is dedicated to helping you meet that challenge through supportive care using the most advanced treatments available. Proton therapy may be a more precise radiation option for treatment of your thoracic cancer to help protect important nearby organs like the heart and normal lung tissue. Our lung cancer specialists will work with you to develop a personalized treatment plan which aims for fewer side effects and improved quality of life.
What We Treat
- Non-small cell lung cancer
- Small cell lung cancer
- Mesothelioma
- Thymoma
- Thymic carcinomas
- Lung metastases
- Mediastinal lymph nodes
- Re-irradiation
Comparison of Proton and X-Ray Therapy
Proton Therapy
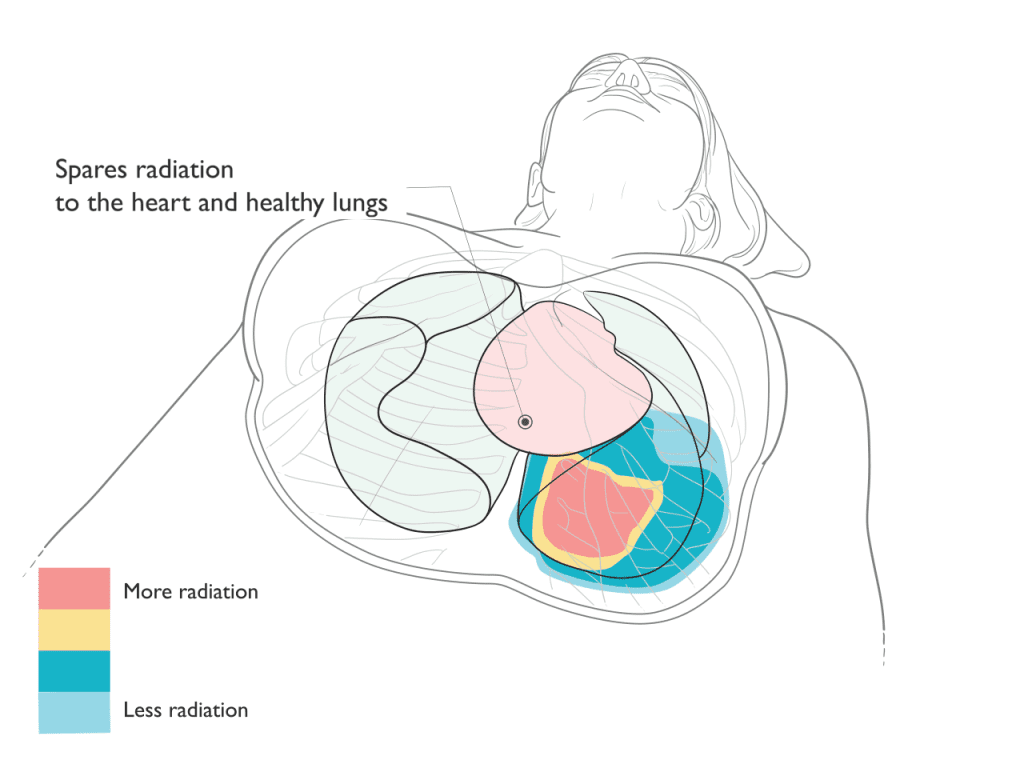
Proton therapy is an extremely precise form of radiation treatment that can often better focus the radiation to match the shape and depth of the target. After treating the target, protons stop, avoiding exit dose radiation through the body. By reducing or avoiding radiation to sensitive normal healthy tissues and organs, proton therapy may reduce some of the side effects that can occur as a result of radiation treatments.
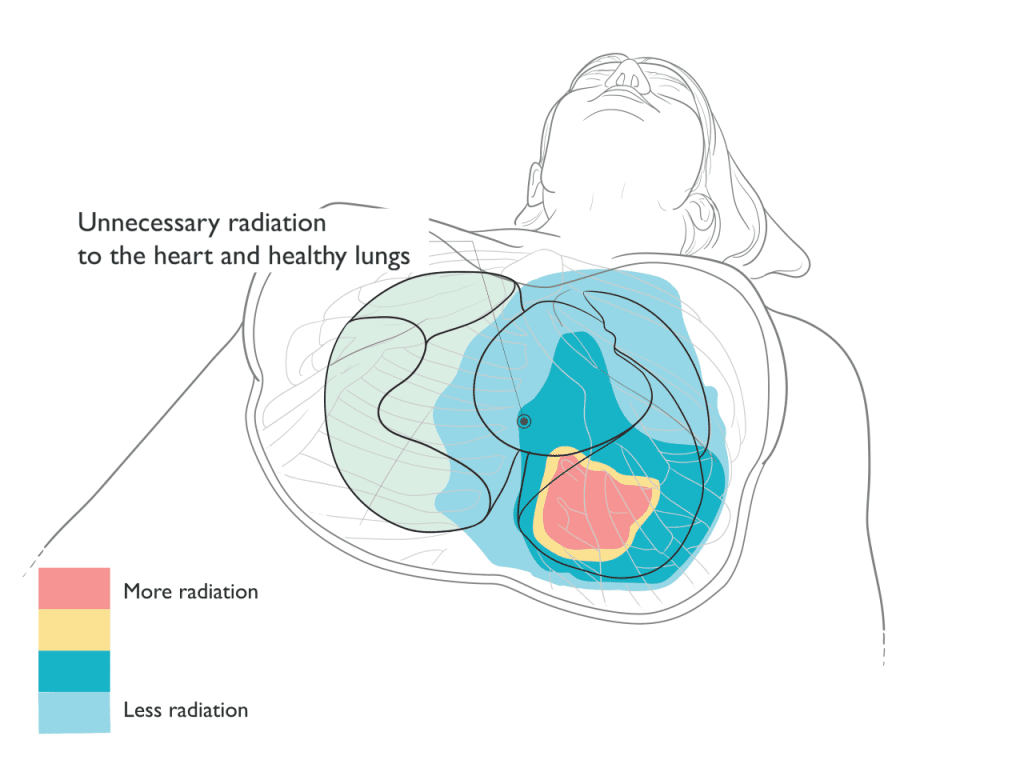
X-Ray Therapy
X-ray based radiation typically requires more beams or angles to deliver the radiation to the target. Unlike proton therapy where the radiation stops at the target, x-rays continue to deliver radiation as they exit through the body. As a result, x-ray based treatments typically result in increased radiation to normal healthy tissues and organs.
Proton Therapy Spares Radiation to the Heart and Lungs
Benefits
In treatment of thoracic tumors, proton therapy can reduce or avoid radiation to surrounding healthy tissue and organs. Depending on the tumor location and type, proton therapy may achieve the following benefits:
- Reduced risk of inflammation of the heart (pericarditis) and future heart problems like hardening of the arteries (atherosclerosis), stiffening of the heart muscle (fibrosis, cardiomyopathy), and heart attacks.
- Reduced risk of inflammation of the lungs (radiation pneumonitis), and problems with lung function (lung fibrosis).
- Reduced risk of difficulty or pain with swallowing (dysphagia or odynophagia) or chronic narrowing of the esophagus (stricture).
- Reducing or radiation to the bone marrow and circulating lymphocytes, which may help support the function of the immune system in taking on fighting cancer.
- Reduced risk of low blood counts (anemia, neutropenia) which may support the body’s tolerance of chemotherapy.
- Reduced risk of developing a future second tumor or cancer, which is most relevant in younger patients, those with a good prognosis and a long life expectancy, and those patients who may have genetic conditions putting them at higher risk for developing other cancers.
Schedule a Consultation
What to Expect with Proton Therapy
The first step in your care is a consultation. During consultation, we review your medical history, perform a physical exam, decide if any additional tests are needed, discuss all radiation options that may be appropriate for your treatment plan, make recommendations, and answer questions.
To plan your treatment, you will undergo a “simulation” or planning session. During this visit our radiation therapists will help position you the way you will be treated each day. A CT scan will be done to create a picture of you in the treatment position to design your radiation plan. It normally takes 10 days for the team to design the proton treatment plan and perform the quality assurance checks before treatment begins.
Proton therapy is typically delivered once daily during weekdays, Monday through Friday. Most patients with thoracic tumors or cancers receive five to six weeks of daily radiation. Some conditions, such as small lung cancers or metastases, can be treated in a shorter period of time such as five treatments over one to two weeks. While some situations are treated with radiation alone, proton therapy may be integrated with surgery, chemotherapy, immunotherapy, or other cancer treatments as part of a comprehensive plan of care.
Like other types of radiation, proton therapy treatments are invisible and painless. Most thoracic tumor treatments average 30 minutes each day in the treatment room. Some tumors in the chest move significantly while breathing. During your radiation planning process, your team will identify the most appropriate methods to manage tumor motion.
Patients are seen by the radiation oncology physician team weekly during treatment to monitor progress, answer questions, address concerns, and manage any side effects from treatment. Your radiation oncologist will discuss a plan to assess response to treatment and for long-term follow-up after therapy.
Studies on Proton Therapy in Thoracic Cancer
Our team has identified these studies as examples of the clinical benefits of proton therapy in thoracic cancer.
Clinical outcomes of image-guided proton therapy for histologically confirmed stage I non-small cell lung cancer
In this prospective phase II clinical trial, 55 patients with early- stage (Stage I, T1a or T1b) non-small cell lung cancer were treated with proton therapy. Thirty-four patients were candidates for removal by surgery but declined that option in favor of proton therapy as a non-invasive treatment. The remaining patients were not medically fit for surgery. At 3 years post-t treatment, the likelihood of treated tumor control after proton therapy was 96%. There were no serious (high grade) side effects noted during or after treatment.
Single Institution Experience of Proton and Photon-based Postoperative Radiation Therapy for Non-small-cell Lung Cancer
This retrospective study examined 136 patients who received radiation therapy after surgery for non-small cell lung cancer. Postoperative radiation for lung cancer is controversial because of concerns about radiation causing toxicities to the heart and lungs. Patients treated with proton therapy had a statistically significantly lower risk of heart toxicities and a trend towards a lower risk of radiation-induced lung inflammation (radiation pneumonitis). Five-year overall survival outcomes favored proton therapy but the difference was not statistically significant in this sample. The radiation dose to the heart and lung were correlated with survival, and proton therapy significantly reduced the average heart and lung dose compared to IMRT.
Proton beam therapy reduces the risk of severe radiation-induced lymphopenia during chemoradiotherapy for locally advanced non-small cell lung cancer: A comparative analysis of proton versus photon therapy
This retrospective study of 223 patients treated with concurrent chemotherapy and radiation for non-small cell lung cancer compared outcomes between those treated with proton therapy and IMRT. Those treated with proton therapy were less likely to develop a severe lymphopenia (depletion of immune cells) which was correlated with the reduced radiation dose to the normal lung tissue. Patients who developed a severe depletion of their lymphocytes had a statistically significantly lower chance of survival at 2-years compared to those who did not. Severe lymphopenia has been associated with reduced overall survival, increased risk of recurrence, and reduced response rates in many cancers.
Bayesian Adaptive Randomization Trial of Passive Scattering Proton Therapy and Intensity-Modulated Photon Radiotherapy for Locally Advanced Non-Small-Cell Lung Cancer
In this randomized phase II trial, patients with non-small cell lung cancer were randomly (flip of the coin) assigned to receive either X-ray or proton radiation delivered together with chemotherapy. The trial found no statistically significant difference in the risk of serious lung inflammation (radiation pneumonitis) or the risk of tumor recurrence between those treated with IMRT or proton therapy. Some believe the trial was negative because older proton technology was used (not pencil beam scanning) but others note that the study design was flawed because it included patients with both newly diagnosed curable disease and patients with metastatic or recurrent disease, as well as including both intact disease and postoperative radiation patients. Furthermore, the trial only included patients for whom both IMRT and proton plans were able to meet the treatment planning goals for normal tissues. Patients for whom proton therapy plans had advantages that could not be met with IMRT were excluded from the trial, removing the patients most likely to benefit from proton therapy.
National Cancer Database Analysis of Proton Versus Photon Radiation Therapy in Non-Small Cell Lung Cancer
This study used the National Cancer Data Base (NCDB) to evaluate survival outcomes for more than 243,000 patients treated with radiation for non-small cell lung cancer between 2004-2012. Fewer than 0.5% received proton therapy. A technique called propensity score matching was used to account for differences in patient characteristics and to minimize selection bias. Treatment with proton beam therapy was associated with better 5-year overall survival in all patients and also in an analysis restricted to patients with stage II and III disease. These outcomes supports further investigation and clinical trials to determine which patients may benefit from proton therapy after accounting for potential patient imbalances not adequately captured by the NCDB.
Comparative Effectiveness of Proton vs Photon Therapy as Part of Concurrent Chemoradiotherapy for Locally Advanced Cancer
This retrospective study examined nearly 1500 patients receiving chemotherapy and radiation for curable cancers of different disease sites, including lung cancers. A technique called propensity score weighting was used to account for differences in patient characteristics (patients treated with proton therapy tended to be older and to have a greater number of other serious health problems) and to minimize selection bias. Patients treated with proton therapy were significantly less likely to have a serious side effect in the first 90 days after treatment, and less often experienced a decline in their overall condition (performance status) during treatment. Patients treated with proton therapy were less likely to have an unplanned hospitalization.
Patient Stories
“I’ve been through it, and I can’t say enough about the amazing care I received. The team who handled my treatments was absolutely wonderful, making a difficult time so much easier to navigate.”

My experience at Emory was incredible—it was as easy as drinking water! The therapy sessions only took about 5 to 10 minutes, and right after, I’d go for a 4-mile walk every single day. I had no side effects whatsoever—I can’t even tell that I had the treatment. Emory truly saved my life, and I couldn’t be more grateful.

Stephen, a 36-year old father from Columbus, Georgia, is one of the almost 2000 patients who have been treated at the Emory Proton Therapy Center since it opened in December 2018. He completed six weeks of proton therapy to treat a brain tumor.

“I went through 37 treatments for prostate cancer at the Emory Proton Center two years ago. The care I received from their team of professionals was amazing. I was willing to travel from South Carolina for treatment, and I’m so thankful I did. I started this fight in 2017 and today my PSA is still undetectable. Truly amazing folks.”

Proton therapy gave Zack his best shot at treating a spinal tumor that had come back. Zack was one of the first patients treated at the Emory Proton Therapy Center after it opened in 2018. The treatments, every weekday for six weeks, took less than one hour of his day and gave Zack the greatest odds of a long life with his wife and children.

Tony was diagnosed with prostate cancer in 2019 and sought care from experts at Emory Proton Therapy Center. He’s confident that the advanced radiation therapy gave him the best cancer treatment possible and says the comfort and care he got from Winship doctors and staff were unmatched. “There were many great solutions here in Atlanta, but the best to me was Emory Proton Therapy Center,” says Tony.