Proton Therapy for Prostate Cancer
A prostate cancer diagnosis can be one of the biggest challenges you and your family will ever face. Our team is dedicated to helping you meet that challenge through supportive care using the most advanced prostate radiation treatments available. Proton therapy is a highly effective and extremely precise radiation option for treatment of prostate cancer to help protect the function of important nearby organs like the rectum, bladder, and bowels, as well as reducing the risk of developing future cancer. Our prostate cancer specialists will work with you to develop a personalized treatment plan that aims for fewer side effects and improved quality of life.
Prostate Cancer Treatment Overview
A prostate cancer diagnosis can be one of the biggest challenges you and your family will ever face. Our team is dedicated to helping you meet that challenge through supportive care using the most advanced prostate radiation treatments available. Proton therapy may be a more precise radiation option for treatment of your prostate cancer to help protect the function of important nearby organs like the rectum, bladder, and bowels, as well as reducing the risk of developing a future cancer. Our prostate cancer specialists will work with you to develop a personalized treatment plan which aims for fewer side effects and improved quality of life.
Types of Prostate Cancer We Treat
- Prostate adenocarcinoma (the most common type of prostate cancer)
- Recurrent prostate cancer after surgery (post-prostatectomy adjuvant or salvage)
- Prostate sarcomas
- Prostate small cell carcinoma
- Pelvic lymph node metastases (prostate cancer that spreads or recurs in lymph nodes)
- Re-irradiation
Benefits of Proton Therapy for Prostate Cancer
In prostate radiation treatments, proton therapy reduces or completely avoids radiation to surrounding healthy tissue and organs. Depending on the tumor location and type, proton therapy may achieve the following benefits:
- Reduced risk of frequent urination or stinging or burning with urination during treatment or of chronic urinary problems after treatment.
- Reduced risk of nausea and diarrhea during treatment.
- Reduced risk of diarrhea and rectal soreness (proctitis) during treatment and of chronic rectal problems after treatments such as rectal bleeding or ulceration.
- Reduced radiation to the bone marrow and circulating lymphocytes, which may help support the function of the immune system in taking on cancer.
- Reduced risk of developing a future second tumor or cancer, which is most relevant in younger patients, those with a good prognosis and a long-life expectancy, and those patients who may have genetic conditions putting them at higher risk for developing other cancers.
What to Expect With Proton Therapy
The first step in your care is a consultation. During consultation, we review your medical history, perform a physical exam, decide if any additional tests are needed, discuss all radiation options that may be appropriate for your treatment plan, make recommendations, and answer questions.
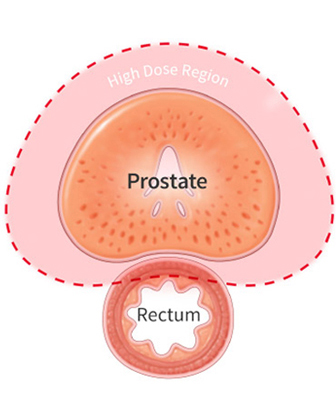
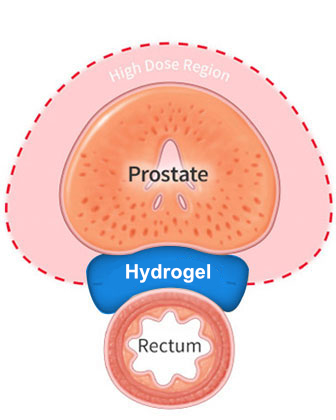
Patients with prostate cancer typically undergo a minor procedure to place three small markers in the prostate, called fiducial markers. These markers allow the treatment team to accurately align the treatment each day to the location of the prostate. Your doctor will also determine if you are eligible for placement of a unique hydrogel between the prostate and rectum (Space OAR® or Barrigel®), which creates additional space between the prostate and the rectum to further reduce radiation exposure to the rectum and dissolves after a few months.
After placement of the markers (and the hydrogel if applicable), most patients return another day for a “simulation” or planning session. During this visit, our radiation therapists will help position you in the way you will be treated each day. A CT scan will be done to create a picture of you in the treatment position to design your radiation plan. Some patients also undergo an MRI during this visit to help identify the target for treatment. It usually takes ten days for the team to design the proton treatment plan and perform the quality assurance checks before treatment begins.
Depending on the stage and other factors, proton therapy for prostate cancer may be delivered over two weeks, six weeks, or eight weeks of treatment. Typically, radiation is given once daily on weekdays, Monday through Friday. For those receiving just five treatments, proton therapy may be delivered every other day. While some situations are treated with proton therapy alone, depending on the stage of the cancer, Gleason score, PSA level, and other factors, proton therapy may be combined with androgen deprivation (hormone therapy) or prostate brachytherapy (internal radiation). Proton therapy may also be used in patients who have had surgery or other cancer treatments as part of a comprehensive plan of care.
Like other types of radiation, proton therapy treatments are invisible and painless. Most prostate treatments average 15-30 minutes each day in the treatment room.
Patients are seen by the radiation oncology physician team weekly during treatment to monitor progress, answer questions, address concerns, and manage any side effects from treatment. Your radiation oncologist will discuss a plan to assess your response to treatment and for long-term follow-up after therapy.
Comparison of Proton and X-Ray Therapy
Proton Therapy
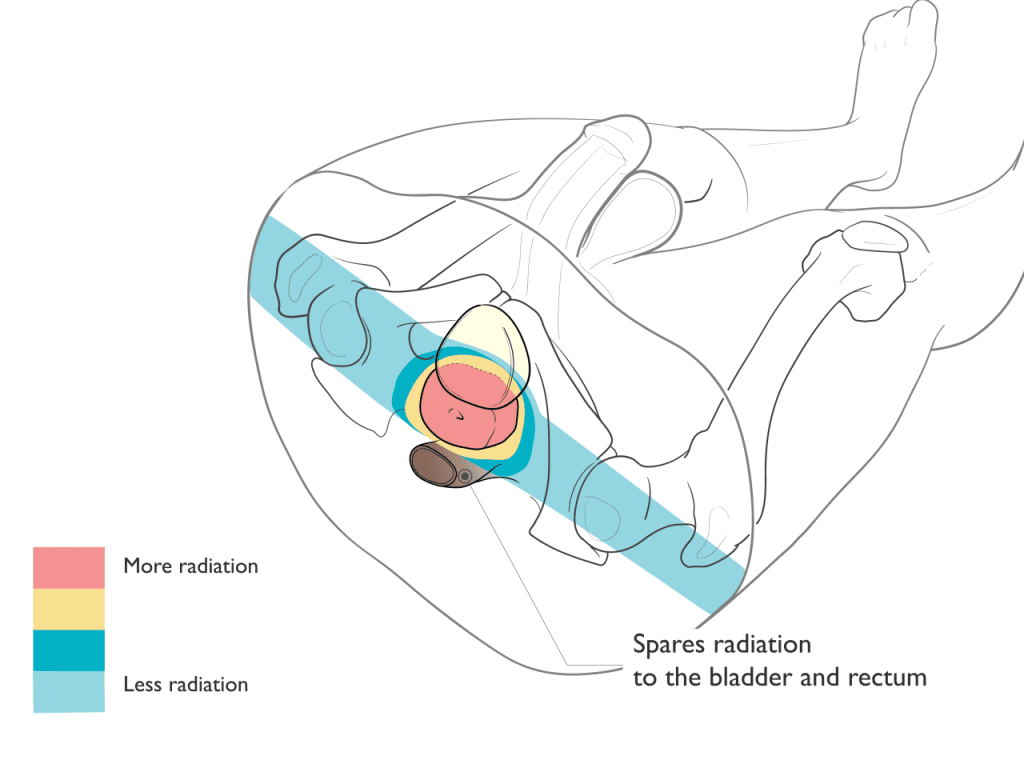
Proton therapy is an extremely precise form of radiation treatment that can often better focus the radiation to match the shape and depth of the target. After treating the target, protons stop, avoiding exit dose radiation through the body. By reducing or avoiding radiation to sensitive, normal, healthy tissues and organs, proton therapy may reduce some of the side effects that can occur as a result of radiation treatments.
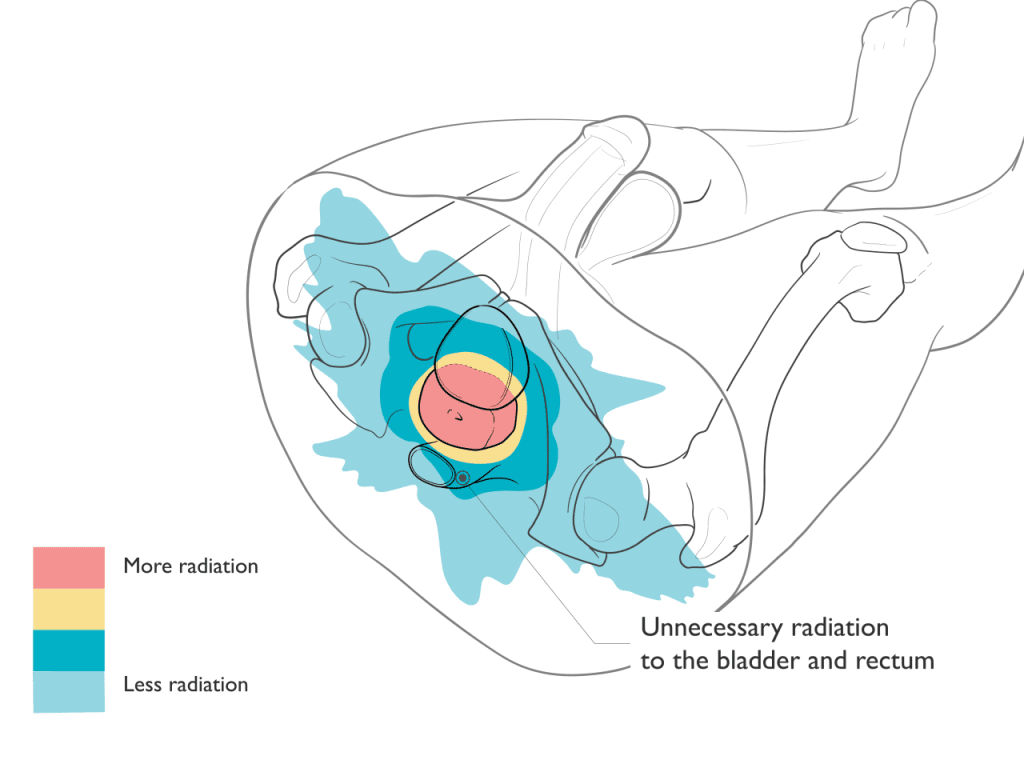
X-ray Therapy
X-ray-based radiation typically requires more beams or angles to deliver the radiation to the target. Unlike proton therapy where the radiation stops at the target, X-rays continue to deliver radiation as they exit through the body. As a result, X-ray-based treatments typically result in increased radiation to normal healthy tissues and organs.
Proton Therapy Spares Radiation to the Bladder and Rectum
Hydrogel: Reducing Radiation Exposure
The prostate and rectum are located very close to each other and are separated only by a small space. When undergoing proton therapy for prostate cancer, your doctor will determine if you are eligible for placement of a unique hydrogel between the prostate and rectum (SpaceOAR® or Barrigel®). The hydrogel creates additional space between the prostate and the rectum to reduce radiation exposure to the rectum further, thereby minimizing unwanted side effects and potential injury to the rectum during treatment.
The hydrogel is placed in a minimally invasive procedure done within our center, and the remains inside the body throughout treatment. The biocompatible gel naturally dissolves after a few months and is cleared in your urine.
Schedule a Consultation
Not All Prostate Cancer Is the Same
When you are first diagnosed with prostate cancer, a natural response is to wonder, “How severe is it?” During consultation, our radiation oncologists evaluate several factors to perform a “risk stratification” of prostate cancer. Risk stratification of prostate cancer relates to the prognosis (how bad is it; how likely is the cancer to spread or recur), guides recommendations on management, and identifies which treatment plans are most likely to cure the cancer.
IMPORTANCE OF CONSULTATION
Understanding a prostate cancer diagnosis can be overwhelming. There are many medical terms, different tests and procedures, and many treatment options to consider! If you meet with one of our expert prostate radiation oncologists in consultation, they will help you to cut through the clutter and focus on what’s relevant to your care. During consultation, we also want to answer your questions, review your treatment options, address your concerns, and understand your desires. The best treatment plan is one that aligns with your preferences and goals.
Understanding Risk Stratification
Several factors are used for prostate cancer risk stratification, some of which are discussed below.
Prostate Specific Antigen (PSA) is a cornerstone of prostate cancer, used in screening, risk stratification, and disease surveillance. PSA is a protein made by prostate cells (including normal and cancerous prostate cells) and is detected in a blood sample.
PSA FOR SCREENING
PSA is not a perfect screening test, but a low PSA level < 4 ng/mL has typically been considered “normal” with a low risk for prostate cancer. A higher PSA level can lead to further tests to look for prostate cancer. Guidelines have changed over time about whether and when men should have a PSA screening test for prostate cancer. According to the US Preventive Services Task Force, men aged 55 to 69 years old should participate in a shared decision with their medical provider about whether to undergo a PSA screening, weighing the potential benefits of early diagnosis against the potential harms of “false alarms” or eventual diagnosis and treatment of low-risk prostate cancer which may never have needed treatment at all.
PSA FOR RISK STRATIFICATION
Once a prostate cancer diagnosis is confirmed, the PSA level is one important component used to understand the risk stratification of the prostate cancer. A PSA < 10 ng/mL is a favorable or low risk value, a PSA of 10 – 20 ng/mL is an intermediate value, and a PSA > 20 ng/mL is a high-risk value. However, PSA needs to be evaluated in combination with other factors to understand the risk level of the cancer and the best treatment options.
PSA FOR TREATMENT RESPONSE ASSESSMENT
Finally, PSA is used to assess response to therapy. The term “biochemical control” refers to when the PSA values are consistent with no active cancer after treatment. At the same time “biochemical failure” or “biochemical relapse” refers to occasions when the PSA rises above a threshold level after treatment and may indicate a recurrence of cancer.
OTHER PSA EVALUATIONS
PSA density refers to the total PSA divided by the size (volume) of the prostate. A higher PSA can simply be a by-product of having a larger prostate gland, which is a common side effect of normal aging, also known as benign prostatic hyperplasia (BPH). So, a higher PSA value in a small prostate gland is more worrisome than the same value in a bigger prostate gland. PSA velocity refers to how quickly the PSA is changing over time. A rapid rise in PSA is more concerning than a slow rise.
Gleason Score and Grade Group refer to the appearance of the cancer cells identified on a prostate biopsy. The Grade Group or Gleason Score is a key factor that guides recommendations about your treatment plan.
- Grade Group 1 = Gleason 6 (or less). Cancer cells look very similar to healthy cells and are considered low-grade. This is the most favorable risk of prostate cancer.
- Grade Group 2 = Gleason 3+4=7. There are mainly low-grade cells but with some more aggressive cancer cells. Often called “favorable intermediate,” the prognosis for cure is still very good.
- Grade Group 3 = Gleason 4+3=7. There are more aggressive cancer cells but still some low-grade cells too. Often called “unfavorable intermediate.”
- Grade Group 4 = Gleason 8. The cancer cells are more aggressive.
- Grade Group 5 = Gleason 9-10. These are the most aggressive prostate cancers, more likely to grow quickly and spread.
Staging (the TNM system) refers to an evaluation of the primary prostate Tumor (“T”), lymph Nodes (“N”) and whether the cancer has spread elsewhere in the body (Metastasis “M”). You may have a clinical T stage (written as cT) if you have not undergone surgery to remove the prostate or a pathologic T stage (pT) if you have undergone surgery to remove the prostate. Clinical T stage is based on a digital rectal exam (DRE) to determine whether the cancer can be felt in the prostate. For many men, the cancer cannot be felt (cT1c), while for others, there may be a hard nodule felt on the prostate (cT2), or in more advanced disease, one may be able to feel the cancer extending outside the confines of the prostate gland (cT3).
Genomic or molecular testing refers to specialized testing that may be performed on a prostate biopsy or the tissue removed during prostatectomy. One common brand of genomic testing is the Decipher score, which looks at a panel of gene expression to help predict the risk that prostate cancer may spread elsewhere in the body (distant metastasis). For some men, genomic testing may help guide decisions such as whether to pursue active surveillance or whether and for how long to use androgen deprivation therapy (ADT). Your radiation oncologist can help you understand whether you may need or benefit from the information provided by genetic testing.
Prostate Cancer Risk Groups
The National Comprehensive Cancer Network (NCCN) provides one of the most commonly used risk stratification methods for prostate cancer. Using PSA, Grade Group, the T stage, and other factors, the NCCN has six risk groups:
- Very low risk. Active surveillance is recommended for most patients. Active surveillance involves careful monitoring so that curative treatment may be offered if there are any future signs of the cancer becoming more aggressive. More than half of patients in active surveillance are able to safely avoid treatment for at least 10 years.
- Low risk. Active surveillance is recommended for most patients.
- Favorable intermediate risk. Active surveillance remains an option. Additional tests may help decide whether to pursue treatment rather than active surveillance. Both radiation (including proton therapy) and surgery may be treatment options.
- Unfavorable intermediate risk. Treatment is generally recommended unless advanced age or other medical problems predict a limited life expectancy. Both radiation (including proton therapy) and surgery may be treatment options. Androgen deprivation therapy is likely to be recommended.
- High risk. Treatment is generally recommended. Both radiation (including proton therapy) and surgery may be treatment options. Androgen deprivation therapy is recommended.
- Very high risk. Treatment is generally recommended. Both radiation (including proton therapy) and surgery may be treatment options. Androgen deprivation therapy is recommended.
Prostate Cancer FAQ
Each session typically lasts around 15-30 minutes, and the total treatment duration varies based on the specific prostate cancer case.
Patient Stories
I’ve been through it, and I can’t say enough about the amazing care I received. The team who handled my treatments was absolutely wonderful, making a difficult time so much easier to navigate.

My experience at Emory was incredible—it was as easy as drinking water! The therapy sessions only took about 5 to 10 minutes, and right after, I’d go for a 4-mile walk every single day. I had no side effects whatsoever—I can’t even tell that I had the treatment. Emory truly saved my life, and I couldn’t be more grateful.

Stephen, a 36-year old father from Columbus, Georgia, is one of the almost 2000 patients who have been treated at the Emory Proton Therapy Center since it opened in December 2018. He completed six weeks of proton therapy to treat a brain tumor.

Dusty was diagnosed with prostate cancer, an uncontrolled growth of cells in the prostate gland. Upon further consultation and research, he was treated with proton therapy and is excited to see an advanced form of radiation therapy is available at the Emory Proton Therapy Center.

Proton therapy gave Zack his best shot at treating a spinal tumor that had come back. Zack was one of the first patients treated at the Emory Proton Therapy Center after it opened in 2018. The treatments, every weekday for six weeks, took less than one hour of his day and gave Zack the greatest odds of a long life with his wife and children.

Tony was diagnosed with prostate cancer in 2019 and sought care from experts at Emory Proton Therapy Center. He’s confident that the advanced radiation therapy gave him the best cancer treatment possible and says the comfort and care he got from Winship doctors and staff were unmatched. “There were many great solutions here in Atlanta, but the best to me was Emory Proton Therapy Center,” says Tony.

Studies on Proton Therapy in Prostate Cancer
Our team has identified these studies as examples of the clinical benefits of proton therapy in prostate cancer.
Overall Survival After Treatment of Localized Prostate Cancer With Proton Beam Therapy, External-Beam Photon Therapy, or Brachytherapy
This study used the National Cancer Data Base (NCDB) to evaluate survival outcomes for more than 276,000 patients treated with radiation for curable prostate cancer between 2004-2015. Fewer than 1% received proton therapy. A technique called propensity score matching was used to account for differences in patient characteristics and to minimize selection bias. Treatment with proton beam therapy was associated with better 5-year overall survival than X-ray based external beam, and similar survival compared to brachytherapy. The improvement in overall survival was most pronounced in men 65 years old or younger. It was also noted that the risk of developing a second cancer was much lower in men treated with proton therapy. These outcomes supports further investigation and clinical trials to determine which patients may benefit from proton therapy after accounting for potential patient imbalances not This study used the National Cancer Data Base (NCDB) to evaluate survival outcomes for more than 276,000 patients treated with radiation for curable prostate cancer between 2004-2015. Fewer than 1% received proton therapy. A technique called propensity score matching was used to account for differences in patient characteristics and to minimize selection bias. Treatment with proton beam therapy was associated with better 5-year overall survival than X-ray based external beam, and similar survival compared to brachytherapy. The improvement in overall survival was most pronounced in men 65 years old or younger. It was also noted that the risk of developing a second cancer was much lower in men treated with proton therapy. These outcomes supports further investigation and clinical trials to determine which patients may benefit from proton therapy after accounting for potential patient imbalances not adequately captured by the NCDB.adequately captured by the NCDB.
Five-Year Biochemical Results, Toxicity, and Patient-Reported Quality of Life After Delivery of Dose-Escalated Image-Guided Proton Therapy for Prostate Cancer
This retrospective report examined the outcomes of over 1200 men treated for prostate cancer with favorable, intermediate, or high-risk disease. Treatment was given with or without androgen deprivation (hormone therapy) depending on level of risk. At 5-years after treatment most men were free from progression (based on PSA and exam) … 99% of those with favorable risk disease, 94% of those with intermediate-risk disease, and 74% of those with high risk disease. Fewer than 0.5% of men had a serious gastrointestinal (bowel) toxicity and fewer than 5% of men had a serious urinary toxicity. These results compare very favorably to outcomes reported with IMRT for prostate cancer.
Long-term outcomes in patients treated with proton therapy for localized prostate cancer
This retrospective report examined the outcomes of over 130 men treated for prostate cancer with favorable, intermediate, or high-risk disease. Treatment was given with or without androgen deprivation (hormone therapy) depending on level of risk. At 5-years after treatment most men were free from progression (based on PSA and exam) … 99% of those with favorable-risk disease, 91% of those with intermediate- risk disease, and 66% of those with high-risk disease. Only 1 patient (0.1%) experienced a serious gastrointestinal (bowel) toxicity and 1 (0.1%) a serious urinary toxicity. These results compare very favorably to outcomes reported with IMRT for prostate cancer.
Postoperative or Salvage Proton Radiotherapy for Prostate Cancer After Radical Prostatectomy
This retrospective report examined outcomes of 102 men treated with proton therapy after prior surgery for prostate cancer, with or without androgen deprivation (hormone therapy) depending on level of risk. Most men (89%) were treated as “salvage” due to a rising PSA or known prostate bed recurrence after surgery, while the remainder received “adjuvant” treatment shortly after recovering from surgery because of high- risk pathologic features. For men treated as salvage, at 5-years after proton therapy, the PSA was brought under control in 57%, and in those men treated with adjuvant proton therapy, the PSA was brought under control in 72%. During treatment serious side effects were rare. After treatment, 7% of men experienced a serious urinary toxicity and none experienced a serious bowel toxicity. These toxicity results compare favorably to outcomes reported with IMRT after surgery for prostate cancer. Among all patients, 97% were free from distant metastases (spread of cancer) at 5-years after therapy.
Second cancer risk after primary cancer treatment with three-dimensional conformal, intensity-modulated, or proton beam radiation therapy
This study used the National Cancer Data Base (NCDB) to examine the frequency of developing a second cancer following radiation treatment for 9 different tumor types – including prostate cancers – in 450,373 patients treated with X-rays or proton therapy. After adjusting for differences in patient age, follow-up duration, radiotherapy dose, use of chemotherapy, sociodemographic differences, and other factors, patients treated with proton therapy had a statistically significantly lower risk of developing a secondary cancer than those treated with X-ray therapy. This significant reduction in risk was seen despite the average follow-up time after radiation being only 5 years. The risk of secondary cancers increases with longer follow-up time after radiation, and it is encouraging to see this signal of reduced risk with proton therapy at an early timepoint.