As the only National Cancer Institute-Designated Comprehensive Cancer Center in Georgia, Winship is at the forefront in radiation treatment for brain cancer. Our staff conduct innovative research and clinical trials that transform how these cancers are identified, treated, and survived.
The radiation oncologists at Emory Proton Therapy Center work with the multidisciplinary Brain and Spine team at Winship, which includes experts in neurosurgery, medical neuro-oncology, neuro-radiology, neuro-ophthalmology, neuro-pathology, supportive oncology, dieticians, social workers, physical therapy, and cancer rehabilitation. Your radiation oncologist will work closely with these and other specialists to customize your brain and spine cancer treatment plan and coordinate your every step. We can also partner and coordinate with a patient’s existing care team, whether they are across town or around the world.
Proton Therapy for Brain and Spine
A brain or spine tumor diagnosis can be one of the biggest challenges you and your family will ever face. Our team is dedicated to helping you meet that challenge through supportive care using the most advanced treatments available. Proton therapy may be a more precise radiation option for treatment of your tumor to help protect important functions of the normal brain and spine like thinking and memory, movement and balance, hormone regulation, hearing, and vision. Our brain and spine specialists will work with you to develop a personalized spine or brain tumor radiation treatment plan that aims for fewer side effects and improved quality of life.
Cancers Treated
Benign (non-cancerous)
- Meningioma
- Pituitary adenoma
- Optic nerve sheath tumor
- Optic nerve glioma
- Paraganglioma or Glomus tumor
- Giant cell tumor
- Craniopharyngioma
- Vestibular schwannoma (acoustic neuroma)
- Hemangioblastoma
- Pilocytic astrocytoma
- Myxopapillary ependymoma
- Ganglioglioma, Gangliocytoma
- Pineocytoma
Other brain tumors
- Astrocytoma
- Oligodendroglioma
- Ependymoma
- Neurocytoma
- Pineoblastoma
- Medulloblastoma
- Atypical teratoid / rhabdoid tumor (ATRT)
- Retinoblastoma
- Glioblastoma
- Choroid plexus carcinoma
Skull base and spine cancers
- Astrocytoma
- Oligodendroglioma
- Ependymoma
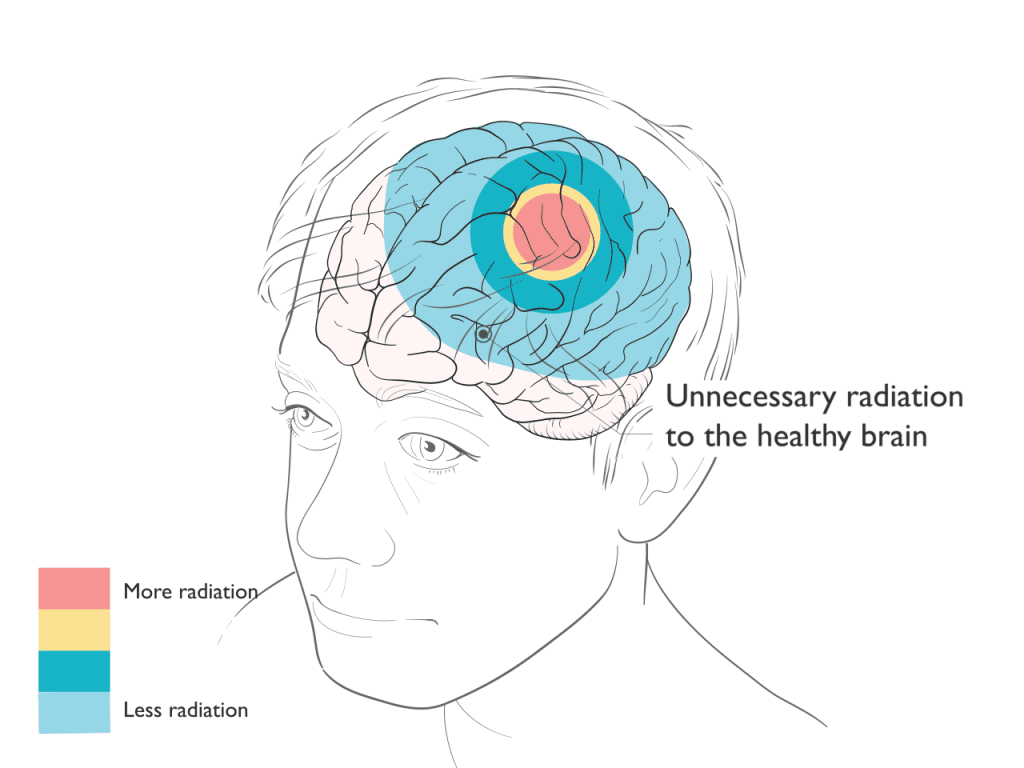
Comparison of Proton and X-Ray Therapy
Proton Therapy
Proton therapy is an extremely precise form of radiation treatment that can often better focus the radiation to match the shape and depth of the target. After treating the target, protons stop, avoiding exit dose radiation through the body. By reducing or avoiding radiation to sensitive normal healthy tissues and organs, proton therapy may reduce some of the side effects that can occur as a result of radiation treatments.
X-Ray Therapy
X-ray based radiation typically requires more beams or angles to deliver the radiation to the target. Unlike proton therapy where the radiation stops at the target, x-rays continue to deliver radiation as they exit through the body. As a result, x-ray based treatments typically result in increased radiation to normal healthy tissues and organs.
Proton Therapy Spares Radiation to the Brain
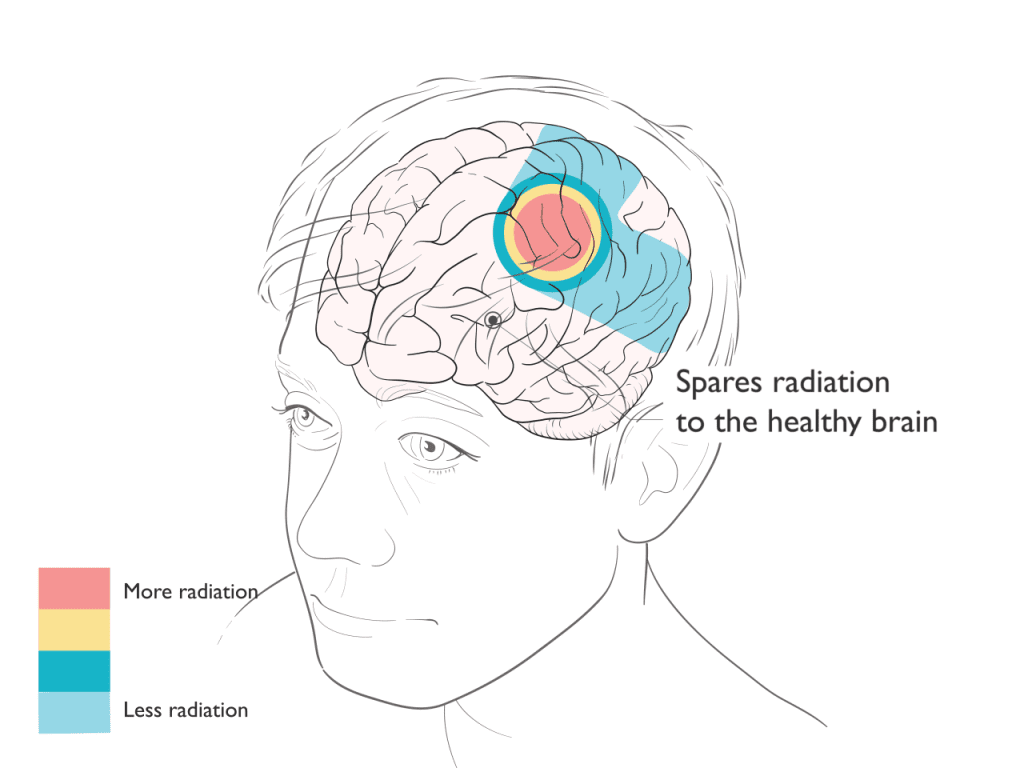
Benefits of Proton Therapy
In treatment of brain tumors and cancer, proton therapy can reduce or avoid radiation to surrounding healthy tissue and organs.
Depending on the tumor location and type, proton therapy may achieve the following benefits:
- Reduction in fatigue, radiation swelling (edema) or injury (necrosis) in normal brain.
- Reduced risk of problems with thinking and memory (neurocognitive deficits).
- Reduced risk of hearing loss after radiation. This is relevant for tumors near the cochlea, such as those in the posterior fossa or temporal lobe.
- Reduced risk of hormone imbalances (endocrine dysfunction) which can particularly affect growth and development in children and young adults. This is relevant for tumors near the pituitary and hypothalamus, such as those in the frontal or temporal lobe.
- Reduced risk of dry mouth after radiation, which can be relevant for tumors nears the parotid glands such as temporal lobe or skull base tumors.
- Reduced or no radiation to the bone marrow and circulating lymphocytes, which may help support the function of the immune system in fighting cancer.
- Reduced risk of developing a future second tumor or cancer, which is most relevant in younger patients, those with a good prognosis and a long life expectancy, and those patients who may have genetic conditions putting them at higher risk for developing other cancers.
In treatment of the spine, the reduction of unnecessary radiation on spine can lead to:
- An improved ability to treat certain tumors that are located near the spinal cord and require a high dose of radiation.
- Reduced risk of inflammation of the heart (pericarditis) and future heart problems like hardening of the arteries (atherosclerosis), stiffening of the heart muscle (fibrosis, cardiomyopathy), and heart attacks. This is relevant for tumors near the heart, for example in the thoracic spine.
- Reduced risk of inflammation of the lungs (radiation pneumonitis) and lung function (lung fibrosis). This is relevant for tumors near the lungs, for example in the thoracic spine.
- Reduced risk of nausea and diarrhea. This is relevant for tumors near the bowels, for example in the lumbar or sacral spine.
- Reduced radiation to the bone marrow and circulating lymphocytes, which may help support the function of the immune system in fighting cancer.
- Reduced risk of low blood counts (anemia, neutropenia) which may support the body’s tolerance of chemotherapy.
- Reduced risk of developing a future second tumor or cancer, which is most relevant in younger patients, those with a good prognosis and a long life expectancy, and those patients who may have genetic conditions putting them at higher risk for developing other cancers.
Schedule a Consultation
What to Expect With Proton Therapy
The first step in your care is a consultation. During consultation, we review your medical history, perform a physical exam, decide if any additional tests are needed, discuss all radiation options that may be appropriate for your treatment plan, make recommendations, and answer questions.
To plan your treatment, you will undergo a “simulation” or planning session. During this visit our radiation therapists will help position you the way you will be treated each day. For patients receiving radiation treatment to the brain, a custom plastic mesh mask is made. This mask helps to get you in the correct position for treatment and fits snugly to remind you to hold still during treatment. You can see and breathe through the mask. A CT scan will be done to create a picture of you in the treatment position to design your radiation plan. Some patients also undergo an MRI during this visit to help identify the target for treatment. It normally takes 10 days for the team to design the proton treatment plan and perform the quality assurance checks before treatment begins.
Proton therapy is typically delivered once daily during weekdays, Monday through Friday. Most patients with brain tumors receive five to six weeks of daily radiation, but some conditions are treated through a shorter course, such as three weeks. While some conditions are treated with radiation alone, proton therapy may be integrated with surgery, chemotherapy, immunotherapy, or other treatments as part of an extensive plan of care.
Like other types of radiation, proton therapy treatments are invisible and painless. Most brain tumor treatments average 30 minutes each day in the treatment room.
Patients are seen by the radiation oncology physician team weekly during treatment to monitor progress, answer questions, address concerns, and manage any side effects from treatment. Your radiation oncologist will discuss a plan to assess response to treatment and for long-term follow-up after therapy.
Studies on Proton Therapy in Brain & Spine Cancer
Our team has identified these studies as examples of the clinical benefits of proton therapy in brain & spine cancer.
A Prospective Phase II Randomized Trial of Proton Radiotherapy vs. Intensity Modulated Radiotherapy for Patients with Newly Diagnosed Glioblastoma
In this small randomized phase II clinical trial, patients with glioblastoma were randomly (flip of the coin) assigned to receive either x-ray or proton radiation delivered together with the drug temozolomide. Compared to those assigned to x-rays, patients treated with proton therapy had a statistically lower rate of fatigue (24% vs. 58%) and on average had fewer toxicities during treatment. The study was not designed to evaluate and did not show a difference in outcome, and there was no significant difference in the average time until patients experienced a cognitive decline. This may be related to the unfortunate poor prognosis of glioblastoma, and suggests patients with more favorable types of glioma with longer survival time may be more likely to benefit from proton therapy.
Proton therapy reduces the likelihood of high-grade radiation-induced lymphopenia in glioblastoma patients: phase II randomized study of protons vs photons
In the same randomized phase II clinical trial as above, patients with glioblastoma were randomly (flip of the coin) assigned to receive either x-ray or proton radiation delivered together with the drug temozolomide. Compared to those assigned to x-rays, patients treated with proton therapy were statistically less likely to develop a severe lymphopenia (depletion of immune cells) which was correlated with the reduced radiation dose to the normal brain. Although the study was not designed to evaluate and did not show a difference in outcome, severe lymphopenia has been associated with reduced overall survival, increased risk of recurrence, and reduced response rates in many cancers.
Proton therapy for selected low grade glioma patients in the Netherlands
This review article discusses the evidence for proton therapy in treatment of patients with low grade gliomas. Because these patients can live a long time, the effect of radiation on neurocognitive function (thinking and memory) is a major concern. Recognizing that proton therapy can provide equivalent efficacy to the tumor with less radiation exposure to the brain, the Dutch National Health Care Institute concluded that there is scientific evidence to assume that proton therapy can have clinical benefit by reducing radiation-induced brain damage. Therefore, their national health care system covers treatment with proton therapy for patients with low grade gliomas who are expected to have a good prognosis and good clinical and neurocognitive function prior to radiation.
Superior Intellectual Outcomes After Proton Radiotherapy Compared With Photon Radiotherapy for Pediatric Medulloblastoma
This retrospective study of 79 children evaluated the change in intellectual test scores over time after treatment for medulloblastoma with craniospinal radiation using protons versus x-rays. Adjusting for differences in patient populations, those treated with protons had superior long-term outcomes in global intelligence quotient (IQ), perceptual reasoning, and working memory compared to those treated with x-rays.
Patterns of Failure Among Patients With Low-grade Glioma Treated With Proton Radiation Therapy
This retrospective study of 141 patients treated with proton therapy for low grade gliomas looked at the 42 patients who eventually developed tumor progression to evaluate the location of tumor progression compared to the volume which was treated with proton therapy. Similar to treatment with x-ray therapy, most tumor progressions occurred within the radiation target, with few “marginal” recurrences occurring at the edge or just outside of the target. Sometimes people erroneously state that proton therapy may be “too precise” for gliomas resulting in more marginal recurrences. This study shows no apparent increase in the risk of marginal recurrences and does not support benefit to patients from having large areas of nontarget normal brain receiving low dose radiation with x-rays.
Proton vs. Photon Radiation Therapy for Primary Gliomas: An Analysis of the National Cancer Data Base
This study used the National Cancer Data Base (NCDB) to evaluate survival outcomes for more than 49,000 patients treated with radiation for World Health Organization (WHO) grade I-IV glioma between the years of 2004-13. Fewer than 0.5% received proton therapy. A technique called propensity score weighting was used to account for differences in patient characteristics and to minimize selection bias. Patients treated with proton therapy were found to have superior average and 5-year survival outcomes than those treated with x-rays and supports further investigation and clinical trials to determine which patients may benefit from proton therapy after accounting for potential patient imbalances not adequately captured by the NCDB.
Comparative Effectiveness of Proton vs Photon Therapy as Part of Concurrent Chemoradiotherapy for Locally Advanced Cancer
This retrospective study examined nearly 1500 patients receiving chemotherapy and radiation for curable cancers of different disease sites, including brain tumors. A technique called propensity score weighting was used to account for differences in patient characteristics (patients treated with proton therapy tended to be older and to have a greater number of other serious health problems) and to minimize selection bias. Patients treated with proton therapy were significantly less likely to have a serious side effect in the first 90 days after treatment, and less often experienced a decline in their overall condition (performance status) during treatment. Patients treated with proton therapy were less likely to have an unplanned hospitalization.
Second cancer risk after primary cancer treatment with three-dimensional conformal, intensity-modulated, or proton beam radiation therapy
This study used the National Cancer Data Base (NCDB) to examine the frequency of developing a second cancer following radiation treatment for 9 different tumor types – including brain tumors – in 450,373 patients treated with x-rays or proton therapy. After adjusting for differences in patient age, follow-up duration, radiotherapy dose, use of chemotherapy, sociodemographic differences, and other factors, patients treated with proton therapy had a statistically significantly lower risk of developing a secondary cancer than those treated with x-ray therapy. This significant reduction in risk was seen despite the average follow-up time after radiation being only 5 years. The risk of secondary cancers increases with longer follow-up time after radiation, and it is encouraging to see this signal of reduced risk with proton therapy at an early timepoint.
Patient Stories
“I’ve been through it, and I can’t say enough about the amazing care I received. The team who handled my treatments was absolutely wonderful, making a difficult time so much easier to navigate.”

My experience at Emory was incredible—it was as easy as drinking water! The therapy sessions only took about 5 to 10 minutes, and right after, I’d go for a 4-mile walk every single day. I had no side effects whatsoever—I can’t even tell that I had the treatment. Emory truly saved my life, and I couldn’t be more grateful.
Stephen, a 36-year old father from Columbus, Georgia, is one of the almost 2000 patients who have been treated at the Emory Proton Therapy Center since it opened in December 2018. He completed six weeks of proton therapy to treat a brain tumor.

“I went through 37 treatments for prostate cancer at the Emory Proton Center two years ago. The care I received from their team of professionals was amazing. I was willing to travel from South Carolina for treatment, and I’m so thankful I did. I started this fight in 2017 and today my PSA is still undetectable. Truly amazing folks.”

Proton therapy gave Zack his best shot at treating a spinal tumor that had come back. Zack was one of the first patients treated at the Emory Proton Therapy Center after it opened in 2018. The treatments, every weekday for six weeks, took less than one hour of his day and gave Zack the greatest odds of a long life with his wife and children.

Tony was diagnosed with prostate cancer in 2019 and sought care from experts at Emory Proton Therapy Center. He’s confident that the advanced radiation therapy gave him the best cancer treatment possible and says the comfort and care he got from Winship doctors and staff were unmatched. “There were many great solutions here in Atlanta, but the best to me was Emory Proton Therapy Center,” says Tony.